Case Report
Benign Fibrous Histiocytoma of Distal Tibia Mimicking Giant Cell Tumor: Case Report
Rashmi Sudhir, Sudha Murthy[1], Koppula Veeraiah Chowdhary
Departments of Radiology and Pathology[1],
Banjara Hills, Hyderabad, India-500034
ABSTRACT
Benign fibrous histiocytoma (BFH) is well-known tumor that typically occurs in soft tissues, with very few cases occurring in bone documented in literature. We report a case of BFH in distal tibia in a 33-year-old woman, who presented with gradually progressing pain and swelling in left ankle. We report the clinical, radiological and histological findings of the case with a brief review of literature.
Introduction
Benign fibrous histiocytoma (BFH) is a mesenchymal tumor with histological features similar to those of xanthofibromas, which include fibrous cortical defect and non-ossifying fibroma, but with different clinical and radiological features.[1] They are characterized by spindle-shaped fibroblasts and histiocytes with few multinucleated giant cells. These lesions are seen in mature bones, with approximately 40% in long bones, mainly around the knee joint and 25% in pelvic bone. However, they can be found virtually in any bone. In long bones, they are positioned in epiphysis or diaphysis with or without metaphyseal involvement.[2]
Case Report
A 33-year-old woman presented with gradual onset of pain and swelling in the left ankle of two months duration. Past medical history and review of systems were noncontributory. On examination, there was a firm, tender, non-pulsatile fixed swelling along distal left tibia with normal range of movement in the ankle joint. Rest of the physical examination was normal.
Biochemical and hematological parameters were within normal limit. Anteroposterior and lateral radiographs of ankle revealed a well defined expansile central lytic lesion with cortical thinning in subarticular region of distal tibia, measuring 7 x 6 cm with coarse internal trabeculations, minimal marginal sclerosis and narrow zone of transition. (Fig. 1) There was no definable matrix mineralization or periosteal reaction . On MRI , mass was hypointense on T1 weighted (Fig. 2A and B), intermediate signal intensity on T2 weighted (Fig.2 C and D) and hyperintense on STIR sequence (Fig.2E) with marginal sclerosis having low signal intensity. There were few intralesional hemorrhagic foci which were hyperintense on T1 and T2 weighted imaging. There was a large cortical defect along the anterolateral and posterior border through which an exophytic component of tumor was extending into the soft tissue (Fig.2E). Minimal soft tissue edema was present, however there was no muscle infiltration.
Aggressive features including destruction with cortical breakthrough and soft tissue mass required tissue diagnosis prior to the surgery to exclude malignancy. Based on the above radiographic appearance, differential diagnosis included giant cell tumor (GCT), aneurysmal bone cyst, brown tumor of hyperparathyroidism and malignant fibrous histiocytoma. Patient’s serum calcium and parathormone levels were within normal levels.
Patient underwent wide local excision of the mass with curettage and bone grafting.
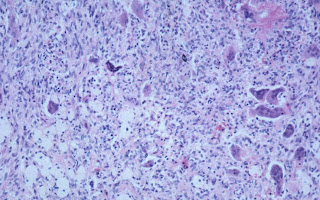
Final histopathology revealed spindle shaped fibroblasts in storiform arrangement admixed with few multinucleated giant cells, foamy histiocytes and hemorrhagic foci (Fig..3). There were no cellular atypia, mitotic activity or pleomorphism. The adjacent skeletal muscles were not infiltrated. These findings supported a final diagnosis of BFH.
Discussion
BFH is a well known tumor to occur in the soft tissue, but is exceedingly rare in bone with very few cases documented in literature.[1] Histologically, BFHs are similar to non-ossifying fibroma and metaphyseal fibrous cortical defect, which are seen in the first two decades of life, and are usually asymptomatic unless associated with a pathological fracture.[2] Benign fibrous histiocytomas are usually seen in relatively older age group, mostly in the third decade of life, with local pain as the chief presenting complaint.[2,3]
Radiologically, they are well-defined radiolucent medullary defects with no matrix mineralization; however, internal trabeculation may be seen. Marginal sclerosis is seen in two-thirds of cases, best demonstrated on CT-scan.[2] Bone expansion and cortical thinning may be seen in most of the cases, however periosteal reaction and soft tissue involvement are very rare. They are mostly seen in ileum, sacrum or long bones commonly around knee joint. In the long bones, they are of diaphyseal or epiphyseal origin with or without metaphyseal component.[4,5] Occasionally, BFH can be locally aggressive and may recur after curettage.[5,6] In Clarke’s series, there were recurrences in 3 out of 8 patients, of which 2 had amputation.[7]
In a well-defined lytic lesion at the end of long bones with soft tissue component, the closest differential diagnosis is giant cell tumor. Other differential diagnoses, which could be included are non-ossifying fibroma or aneurysmal bone cyst (ABC); but both of them occur in the first or second decade of life. Radiologically, non-ossifying fibromas are usually eccentric corticomedullary lytic lesions with sclerotic margin and confined to the metaphysis. Aneurysmal bone cysts show fluid-fluid levels on MRI . In adults, ABC component can be seen with GCT. [8]
In our patient, the clinical and radiological features favored a diagnosis of locally aggressive giant cell tumor. However, the final histopathologic diagnosis came as benign fibrous histiocytoma. The only radiological feature, which was more in favor of BFH, was presence of. marginal sclerosis which is usually not seen in GCT. Hence, benign fibrous histiocytoma should also be considered as a diagnostic possibility in a patient with clinico- radiological findings suggestive of giant cell tumor, especially if marginal sclerosis is present. Tissue diagnosis should be performed prior to surgery in these cases.
References
1. Al-Jamali J, Jerlach UV, Zajonc H. Benign fibrous histiocytoma of distal radius: A case report and review of literature. Hand Surg. 2010;15:127-9.
2. Kyriakos M. Benign fibrous histiocytoma of bone. Lyon(France): IARC Publication; 2002.p.292-3.
3. Sanatkumar S, Rajagopalan N, Mallikarjunaswamy B, Srinivasalu S. Benign histiocytoma of distal radius with congenital dislocation of radial head. A case report. J Ortho Surg. 2005; 13:83-87.
4. Clark TD, Stelling CB, Fechner RE. Benign fibrous histiocytoma of the left 8th rib. Case report 328. Skeletal Radiol 1985;14:149–51.
5. Destouet JM, Kyriakos M, Gilula LA.
6. Mastuno T. Benign fibrous histiocytoma involving the ends of long bones. Skeletal Radiol 1990;19:561–6.
7. Clarke BE, Xippell JM, Thomas DP. Benign fibrous histiocytoma of bone. Am J Surg Pathol 1985;9:806-15.
8. Unni, KK & Inwards, CY. Dahlin’s bone tumors: General aspects and data on 10,165 cases. Lipincott, Williams & Wilkins, 6th ed 2009.
Fig 2A
Fig 2B
Fig 2A & B: T1- Weighted sagittal and coronal images showing that the lesion is hypointense with small hyperintense area of subacute hemorrhage.
Fig 2D
Fig 2C & D: T2-Weighted sagittal and coronal images show intermediate signal intensity lesion with intralesional hypo and hyperintense hemorrhagic foci and surrounding hypointense sclerotic margin.
Fig 2E: Axial STIR sequence showing that the lesion is hyperintense with cortical defect and large exophytic component of the tumor extending into soft tissue along anterolateral and posterior border of tibia.
Fig 3: Histologic findings reveal spindle shaped fibroblasts admixed with few multinucleated giant cells and foamy histiocytes.
For any comments, please mail me at:
rashmi4210@yahoo.com
For any comments, please mail me at:
rashmi4210@yahoo.com






Good Information. Can you please suugest the best surgeon for the benign fibrous histiocytoma? I need information as soon as possible. My relative have same tumor and recurred twice. Now again it occurred 3rd time. Need a suggestion, who is the best orthopaedic oncologist in India.
ReplyDelete